NOTE: This article is being re-published to keep NYP staff appraised on the tools available to aid them in the ICD-10 transition. The code mapping tools for Cornell and Columbia can be found on the Support Center Page under the ‘Other Resources & Materials’ or by clicking here for Cornell and here for Columbia.
As we approach the October 1st, 2015 cutover date for ICD-10, many departments have requested the ICD-10 equivalents of their most commonly used ICD-9 codes. In response, the ICD-10 Project Management Office has built a dynamic tool that allows users to drill down into the campus, registration area, clinic ID, or even individual physician, view the ICD-9 codes for hospital-based outpatient services based on frequency, and see the ICD-10 codes to which each ICD-9 code can map.
There are two code mapping tools: one for Cornell and one for Columbia. The tools can be downloaded from the ICD-10 AnTENna website, and are available as links under the section on the right side of the page labeled “ICD-9 / ICD-10 Code Mapping Tool.”
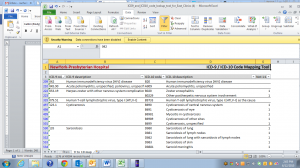
The tools, built in Excel, have two main tabs. The “filters” tab is where the user selects the campus, registration area, clinic ID, and/or physician for which they would like to view results. After the selections are made, the table below updates to show the relevant ICD-9 codes and descriptions, sorted by volume. For each ICD-9 code, the table also displays the number of ICD-10 codes that ICD-9 code can map to. The more ICD-10 codes a given ICD-9 code can map to, the more additional documentation details will be required in ICD-10, and the more focus is warranted as we prepare for the transition. A summary table in the top right shows some key statistics for the selection.
In the “9 to 10 map” tab, users can see the specific ICD-10 codes that their current ICD-9 codes can map to. This report makes it clear which ICD-9 codes map to a single ICD-10 code vs. multiple ICD-10 codes, helping to illuminate the areas where the need for documentation enhancement is greatest. From looking at the descriptions of the ICD-10 codes, users can tell what additional documentation details will be needed in order to ensure that the correct ICD-10 code can be selected.
These tools are part of a larger arsenal of education and communication designed to arm departments with the information they need to be fully prepared for ICD-10. Please reach out to the ICD-10 Project Management Office at ICD-10help@nyp.org if you have any questions.