Written by Dr. Abhishek Jacob
See full article here
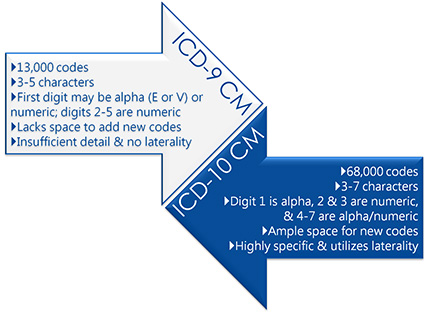
It is common knowledge that ICD-10 CM & PCS code sets will increase granularity, improve axes of classification and provide a more scientific approach to coding, opening up tremendous growth in our understanding of disease conditions and associated treatment protocols.
For the first time in 36 years, we have the opportunity to revamp the clinical terminology being used to measure effectiveness of healthcare services, refine clinical grouping and associated reimbursement methodologies and enhance capability to conduct public health surveillance.
Today’s Challenges
- Many provider organizations believe that because ICD-10 has been characteristically complex to implement and includes many new and potentially amusing codes (e.g. W59.22XD – “struck by turtle, subsequent encounter”), the increased quantity may not be very useful from a treatment and re-imbursement perspective. These issues significantly undermine the potential benefits ICD-10 will have on documenting and reporting clinical conditions, enhancing clinical terminologies and, most importantly, measuring the effectiveness of treatments for better disease surveillance – like the current course of action and treatment during the recent outbreak of Ebola cited later.
- Though a competing priority, Meaningful Use (MU) implementation has a mutual dependency and benefit to ICD-10. One of the most important drivers of meaningful usage of EMR is allowing clinical data to be effectively utilized and shared between EHR systems. To accomplish this objective of using standard clinical terminologies, ICD-10 and MU requirements must be incorporated into EHR systems concurrently. This would help achieve comprehensive system interoperability and shed light on the benefits of a national health information infrastructure. ICD-10 and MU implementation are complimentary and are required to be applied together, and therefore should not be viewed as conflicting priorities.
- Last, rather than being used as a counterpoint to discredit the tremendous potential benefit of ICD-10 implementation, many of the so-called irrelevant codes, such as “struck by turtle, subsequent encounter,” fall in external causes of injury chapter and are not necessarily required for reimbursement of diseases surveillance, which means their usage can be restricted on a case to case basis.
ICD-10: The Next Generation of Clinical Terminology and Coding
ICD-10 holds true promise to expedite a much needed revamp of existing clinical terminologies and coding for high value patient encounters. Below is an analysis of a simple example that compares how ICD-10 provides significant enhancement to our ability to measure healthcare services and how increased sensitivity would assist in refining existing grouping and reimbursement methodology.
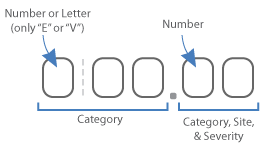
With more than 650,000 procedures per year, angioplasty in one of the most commonly performed operations, contributing approximately $13 billion per year to U.S. healthcare spending. According to a study published in The Journal of the American Medical Association in 2012, almost half of the angioplasties conducted in non-emergency situations may not benefit patients. In ICD-9 CM, angioplasty is represented by only 1 code- 39.50 and since ICD-9 CM lacks the granularity, it might not be possible to relate the clinical outcomes of the procedure with the associated reimbursement.
ICD-9-CM
Angioplasty – 1 code (39.50)
ICD-10-PCS
Angioplasty – 854 codes
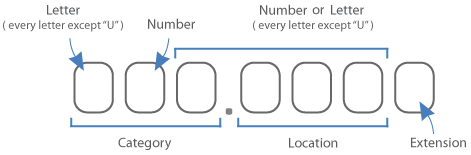
ICD-10 CM not only specifies the body part the procedure was conducted on but also the approach, the device used and the type of stent placed. This granularity allows for correlation between clinical outcomes and a specific type of procedure, thereby improving the overall efficacy of the treatment.
Some examples of ICD-10 granularity of Angioplasty codes include:
- 047K04Z – Dilation of right femoral artery with drug-eluting intraluminal device, open approach
- 047K0DZ – Dilation of right femoral artery with intraluminal device, open approach
- 047K0ZZ – Dilation of right femoral artery, open approach
- 047K34Z – Dilation of right femoral artery with drug-eluting intraluminal device, percutaneous approach
- 047K3DZ – Dilation of right femoral artery with intraluminal device, percutaneous approach
The granularity that comes with ICD-10 is critically important to the future of our healthcare system. The outbreak of Ebola has allowed many analysts and experts in the field to stress how ICD-10 and improved clinical terminology intensifies the need and benefits of the new code set. ICD-10 could allow healthcare providers to measure the effectiveness of treatments for better disease surveillance and outbreak response.
ICD-9 CM has no specific code for reporting Ebola hemorrhagic fever (EHF). The closest match is 065.8 “other specified arthropod-borne hemorrhagic fever.” ICD-10 CM has a specific code, A98.4 “Ebola virus disease.” In ICD-9 CM Ebola is classified under “arthropod-borne viral diseases” whereas in ICD-10 it is classified as “arthropod-borne viral fevers and viral hemorrhagic fevers.”
There is currently no drug or vaccine available to treat Ebola and most of the treatment is based on experimental drugs. Since the outbreaks, until now, have appeared prominently in Africa, where there is a very restricted use of standard clinical terminology and modern EHR systems, little information is available about the natural reservoir host of Ebola virus.
And as we’ve witnessed, because physicians aren’t able to accurately document the causative factors, strains of virus and treatment protocols, our response to the outbreak has been restricted to a tactical stoppage of spread. ICD-9 CM does not have any codes to document Ebola accurately, and though ICD-10 CM has only one code to report Ebola, the ability to expand the categorization in ICD-10 ensures that researchers, authorities and care providers can better prepare for response, resulting in potential lives and millions of dollars saved. This is a classic example of how accurate usage of clinical terminology for disease surveillance associated with ICD-10 implementation holds true promise.
Continued use of ICD-9-CM as a medical code set standard threatens to jeopardize the ability of the U.S. healthcare industry to effectively collect and use accurate, detailed healthcare data and information for the betterment of domestic and global healthcare. Clinical terminology modernization and standardization are amongst the most important steps required to maximize the power of healthcare data and, in doing so, build a better healthcare system for the 21st century.