SUMMARY OF EVENTS
The previous ten days of activity continue to demonstrate the organization’s commitment to and the overall success of the ICD-10 implementation. Since our last update, NYP has received more than 1300 commercial third party payments for inpatient claims coded and billed with ICD-10 codes including the early signs of payment from some of our larger commercial payers such as Blue Cross, Aetna, Cigna, and United Healthcare. Some lingering billing issues, specifically related to what are referred to as “cross-over period” encounters (From dates prior and Through dates after October 1) are being researched and remedies are being tested and implemented. The impact of these issues is nominal in the context of NYP’s overall revenue base. As a reminder, the ICD-10 Support Center’s last day of operations will be Friday, October 30. Providers and staff with inquiries can continue to e-mail ICD-10Help@nyp.org and a member of the project team will respond. An ongoing summary of the project is listed below and the full presentation can be found here.
OVERALL IMPACT
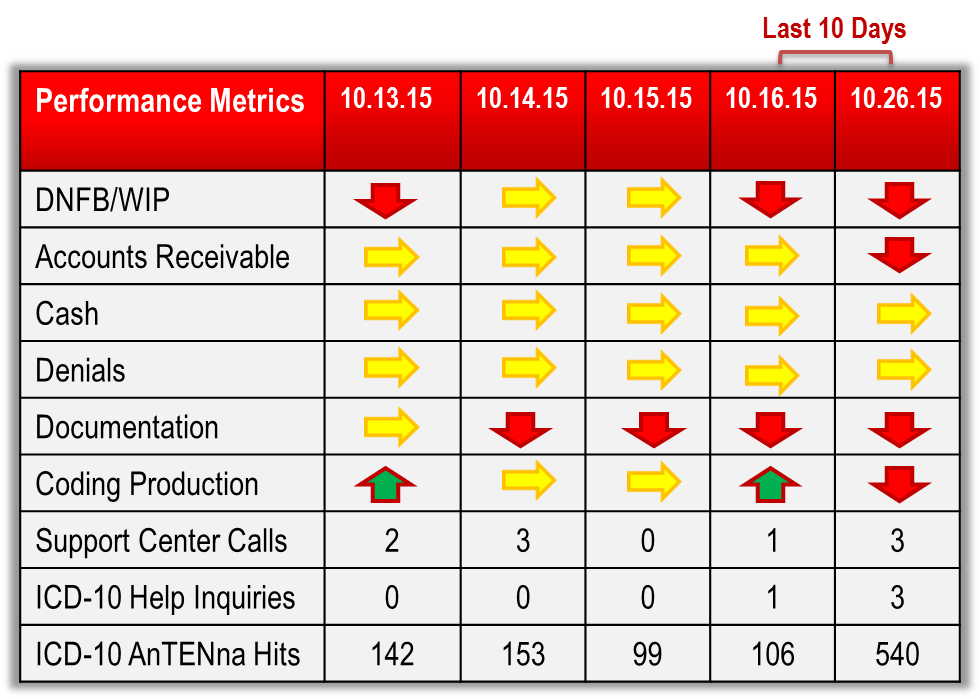
Financial and operating metrics are trending slightly unfavorable in what appears to be largely due to typical productivity ebbs and flows of the operation and not ICD-10 related issues. Providers continue to interact with the new Allscripts documentation assistance tool, ICDx, though actually leveraging it to document in the patient’s record is still somewhat low. As such, Documentation Improvement specialists in HIM continue to generate increased volumes of provider inquiries in an effort to take advantage of the specificity available in ICD-10. Coding production is slightly down due to requests to dual code select populations of inpatient encounters but should return to normal and expected production by month end. Payments for current month discharges are trending similar to previous months suggesting that some insurance carriers are demonstrating an ability to pay under ICD-10.
ITEMS BEING RESOLVED
The Eagle IT team is applying vendor remedies to correct some billing issues related to cross-over period claims and should be resolved before month end. Health Information Management professionals are dual coding select populations of inpatient encounters in order to comply with payer specific billing requirements. An updated implementation issues log can be found here.
SUPPORT CENTER ACTIVITY
The ICD-10 Support Center received 3 phone calls and 3 e-mail inquiries in the last 10 days while preparing for the “Transition back to Operations” webinar on Thursday, October 29. In total, the Support Center has logged 103 issues and 17 remain open. Reference materials and other educational aids continue to be produced and disseminated to the organization. The ICD-10 AnTENna website recorded an additional 540 hits.
REMEMBER
- ICD-10 Diagnosis Codes are 3 – 7 characters, alpha-numeric, and ALWAYS begin with a letter
- ICD-10 is date of service/date of discharge sensitive
- DO NOT insert decimal points when entering ICD-10 diagnosis codes in Eagle
- Use ICDx to assist with documentation efforts in Sunrise Clinical Manager (SCM)
- Correct old health issues by clicking the health issue, selecting ‘update preferred mapping, select the ICD-10 code, and clicking ‘Accept”
- Ambulatory encounters scheduled prior to October 1, 2015 that included ICD-9 diagnosis codes will have to be manually corrected by converting the code to ICD-10 upon arrival.
HELP
For continued assistance and inquiry, please e-mail ICD-10Help@nyp.org, or visit the ICD-10 AnTENna website.