SUMMARY OF EVENTS
Day 13 of the transition did not reveal any bad luck in the form of new issues or challenges and both inpatient and outpatient billing continue to produce expected volumes of claims to third party insurance carriers. Reviews of current unbilled inventories similarly indicate that any billing errors that are occurring are in line with standard operational deficiencies and not ICD-10 related. Call and inquiries to the ICD-10 support center have decreased and systemic issues affecting subsets of encounters have largely been resolved. As such, Support Center troubleshooting operations will begin to subside with remaining efforts concentrated on the monitoring of payment and denial in conjunction with Patient Financial Services (PFS). An ongoing summary of the project is listed below and the full presentation can be found here.
OVERALL IMPACT
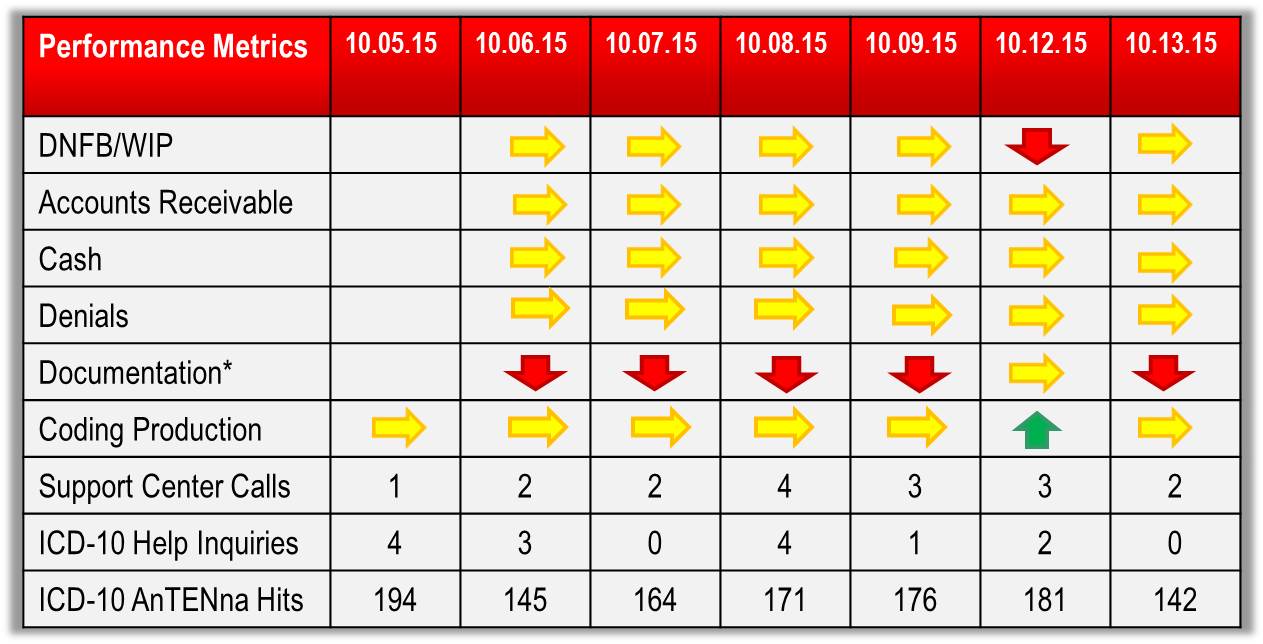
At this stage of the transition, the impact of the ICD-10 transition on patient care/patient experience activities is essentially anon-factor. Financial and operating metrics continue to remain stable as Support Center efforts prevent ICD-10 related issues from funneling back to the operation. Coding production has remained solid despite the transition to the new code set. Documentation Improvement specialists in HIM continue to generate increased volumes of provider inquiries in an effort to take advantage of the specificity available in ICD-10. Providers are demonstrating and uptick in their interaction with new Allscripts documentation assistance tool, ICDx.
ITEMS TO BE RESOLVED
The interface issue between R4 and Eagle has been fixed and 90% of affected cases have been corrected. Similarly, the code dictionary issue in the billing system has been corrected and all affected cases are now scheduled to or have already generated accurate bills. Remaining open items are largely of the “one-off” variety with specific expertise from the Support Center reaching out to providers and staff to resolve. OR Manager team continues to work with its vendor to identify solutions to eliminate invalid code options from its data dictionaries. An updated implementation issues log can be found here.
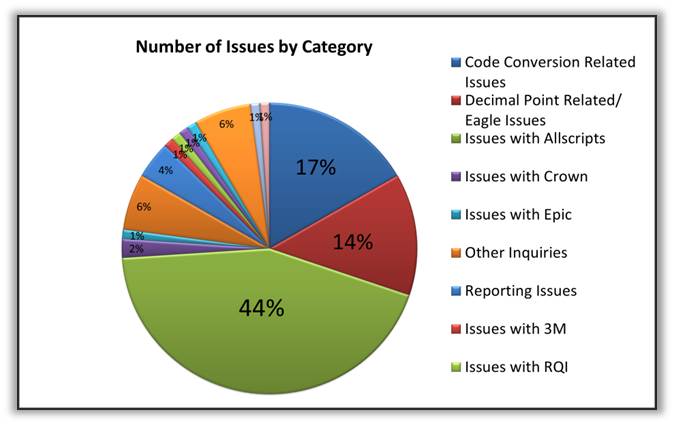
SUPPORT CENTER ACTIVITY
Staff received 2 phone calls and 0 e-mail inquiries while correcting approximately 200 additional outpatient encounters erroneously assigned ICD-9 codes. In total, the Support Center has logged 96 issues and 19 remain open. The ICD-10 AnTENna website recorded an additional 142 hits.
REMEMBER
- ICD-10 Diagnosis Codes are 3 – 7 characters, alpha-numeric, and ALWAYS begin with a letter
- ICD-10 is date of service/date of discharge sensitive
- DO NOT insert decimal points when entering ICD-10 diagnosis codes in Eagle
- Use ICDx to assist with documentation efforts in Sunrise Clinical Manager (SCM)
- Correct old health issues by clicking the health issue, selecting ‘update preferred mapping, select the ICD-10 code, and clicking ‘Accept”
HELP
For continued assistance and inquiry, please call the ICD-10 Support Center at 646-NYP-9-2-10 (646-697-9210), e-mail ICD-10Help@nyp.org, or visit the ICD-10 AnTENna website.