Again, we‘d like to thank all staff and providers who have worked collaboratively with us to make our ICD-10 implementation an overwhelming success. The ICD-10 Support Center is officially closed. In an effort to transition certain ICD-10 specific responsibilities back to the operations ownership, we held an Operational Transition webinar on Thursday, October 29th.
During this session we provided participants with:
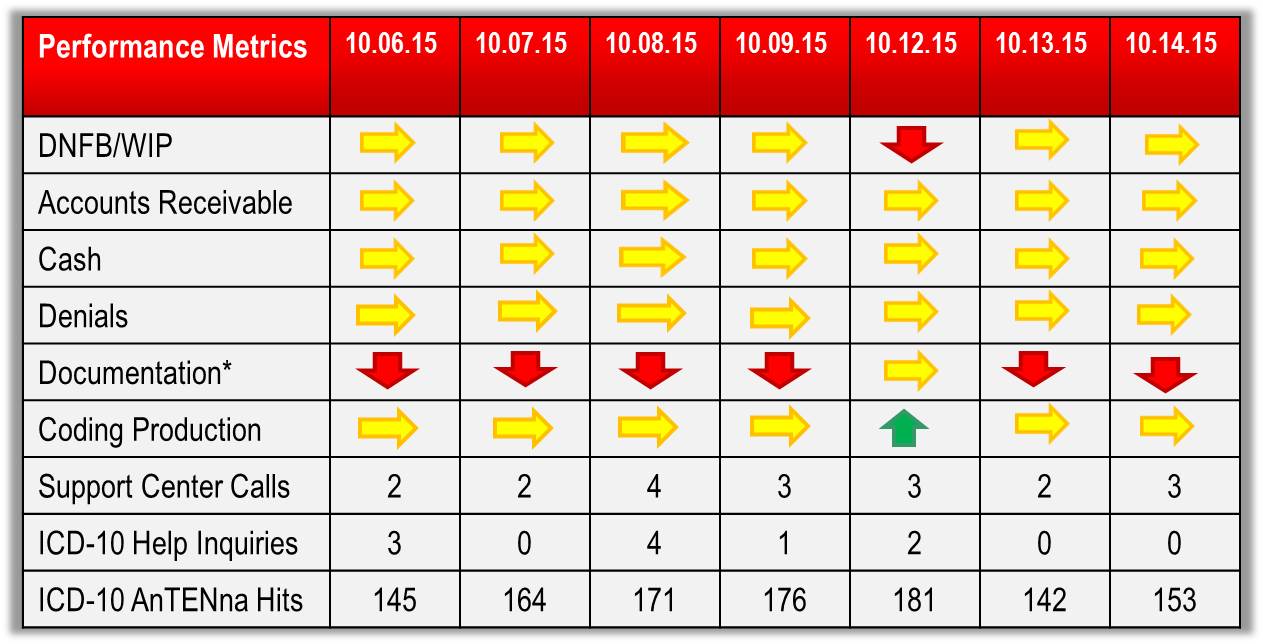
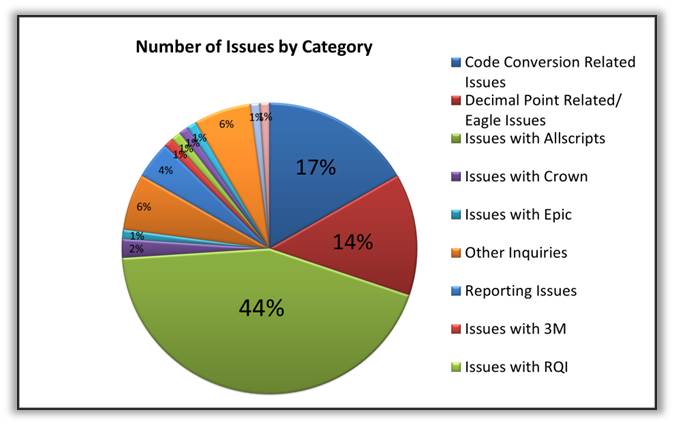
- A current state of implementation performance including key measures of operating and financial success
- A status on any remaining issues and items being resolved and applicable contingency procedures for those items
- A review of the various materials, resources, and tools that will continue to be available to you, your staff, and providers to leverage and support ongoing self-sufficiency in ICD-10
You can find a copy of this presentation here.
For ongoing support regarding the transition to ICD-10 you can e-mail ICD-10Help@nyp.org or visit NYP’s ICD-10 AnTENna website for updates, training aids & other useful resources. Please keep in mind, there will no longer be a telephone line for the Support Center. If you have any IT application related issues, contact the service desk at 212-746-4357 (4-HELP).
We Came, We Saw, We Conquered, I-10!