It is no coincidence that as we head into the Labor Day weekend, that it will take no less than a spirited and workman-like (work person-like) effort by thousands of NYP employees and clinical professionals to ensure our transition to the new ICD-10 coding system is seamless and successful. From previous updates, you are aware that much work has been done through the contributions of more than hundred core project team members and dozens of additional individuals focused on task specific activities to prepare for October 1. Many of those same individuals will be on call to support the Hospital through the ICD-10 transition period defined from September 1, 2015 through November 30, 2015. On behalf of the project and NYP, I extend my advanced appreciation and gratitude for those eventual efforts. However, as we embark on “changing the dictionary” that describes our patients’ conditions and the services we provide to treat those conditions, the ICD-10 project becomes an organization-wide opportunity to leverage an improved classification system for better data, better research, and some day – better patient care. So, with 30 days to go, here is your ICD-10 readiness checklist.
30. Understand changes to enterprise and department specific computer applications and how they impact your operation.
29. Confirm that reports, forms, documents and other data capture vehicles that leverage ICD-9 codes as criteria have been updated to include equivalent ICD-10 codes.
28. Confirm with your IT colleagues that data is interfacing both to and from applications used by your department.
27. Identify equivalent ICD-10 codes for clinical orders spanning the September/October time frame.
26. Communicate and promote the documentation assistance tools available in Crown, Allscripts SCM (ICDx), and Epic (Diagnosis Calculator) with physicians and other providers.
25. Promote and provide the inclusion of additional specificity in clinical documentation including items like acuity, anatomic site, laterality, root procedures, related conditions, disease status and stage, association with medications and/or drug use, causative agents, and significance of abnormal lab values… just to name a few.
24. Encourage physicians and other providers to download the Precyse University apps, ICD10 Doc Talk and ICD10 Mobile Documentation Guide to have valuable ICD-10 information at their fingertips (yes, they’re FREE)!
23. Promote the www.roadto10.org website for physicians. This CMS website is filled with valuable information on specialty specific documentation and coding information including ICD-10 Clinical Concept “cheat sheets”.
22. Review Medicare coverage (e.g. – LCD, NCD) policies for any ICD-10 impact of department/service specific procedures, drugs, tests, and exams.
21. Reduce unbilled receivables focusing on encounters most likely to generate accelerated cash for the Hospital.
20. Ensure appropriate data is available to financially clear cases according to their date of service/date of discharge – Remember, September: 9th month – 9 codes, October: 10th month – 10 codes!
19. Coordinate with non-NYP physicians and providers to ensure ICD-10 codes are provided on referrals.
18. Recognize the visual and structural difference between and ICD-9 and an ICD-10 code.
17. DON’T become a coder – but DO become familiar with codes that are common to your service and your patients.
16. Confirm that registries and external entities with whom you may exchange ICD-10 information are ICD-10 compliant and ready to accept NYP data.
15. Keep an eye out for transition period operating guidance related to revenue cycle operating activities for recurring services (e.g. – physical therapy, behavioral health, chemotherapy, radiation oncology, etc.)
14. Visit the Hospital’s official ICD-10 website, ICD-10 AnTENna often for updates, guidance, and support.
13. Encourage all staff to watch the ICD-10 organizational awareness video, ‘ICD-10: A New Language in Healthcare” available on their transcripts in the NYP Learning Center.
12. Use ICD-10Help@nyp.org to submit inquiries, questions, and issues to the ICD-10 Support Center.
11. Call the ICD-10 Support Center Telephone number: (646) NYP-9-2-10 (or 646-697-9210) – effective September 28, 2015.
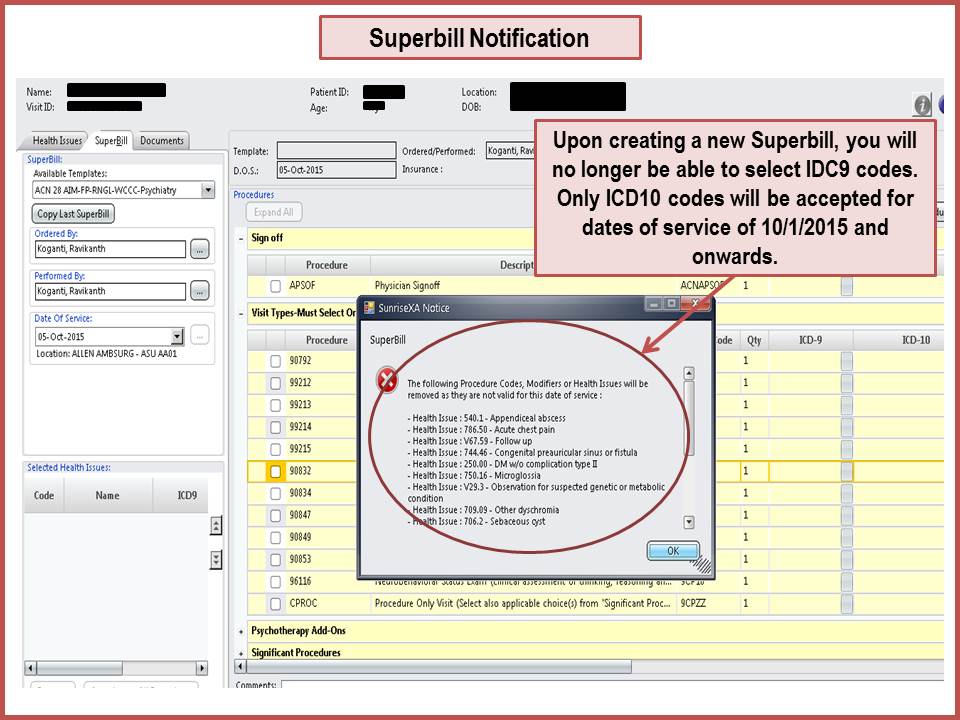
10. Leverage code conversion tools to identify potential ICD-10 options to ICD-9 codes. DO NOT use them to code encounters.
9. DO NOT INCLUDE decimal points when entering ICD-10 codes into the EAGLE registration and billing system.
8. Be prepared to dual code inpatients covered under Medicare part B benefits only that span the September/October time frame (OK – this one is pretty small).
7. Move all interfaces, functionality, and reporting, and operating contingencies into production environments.
6. Integrate ICD-10 conversation into team meetings, staff huddles, and other communication devices – Broad based awareness is our greatest asset.
5. Think through resources and coverage for potential issues that may require remediation such as new registrations, re-entry of codes, re-writing of orders, correction of billing errors, and resubmission of insurance claim denials.
4. Set up monitoring tools to ensure orders, documentation, coding, billing, and payment are producing expected outcomes in ICD-10.
3. Prepare to leverage more specific data on our patients to improve quality, safety, delivery, length of stay, patient flow, costs, meaningful use, medication management, population health, and a lot of other stuff.
2. Be Flexible – issues will arise. It’s how we communicate, triage, troubleshoot, and revolve them that counts.
1. Prepare to celebrate a successful ICD-10 implementation!